UC Irvine researchers harness AI to advance brain cancer research
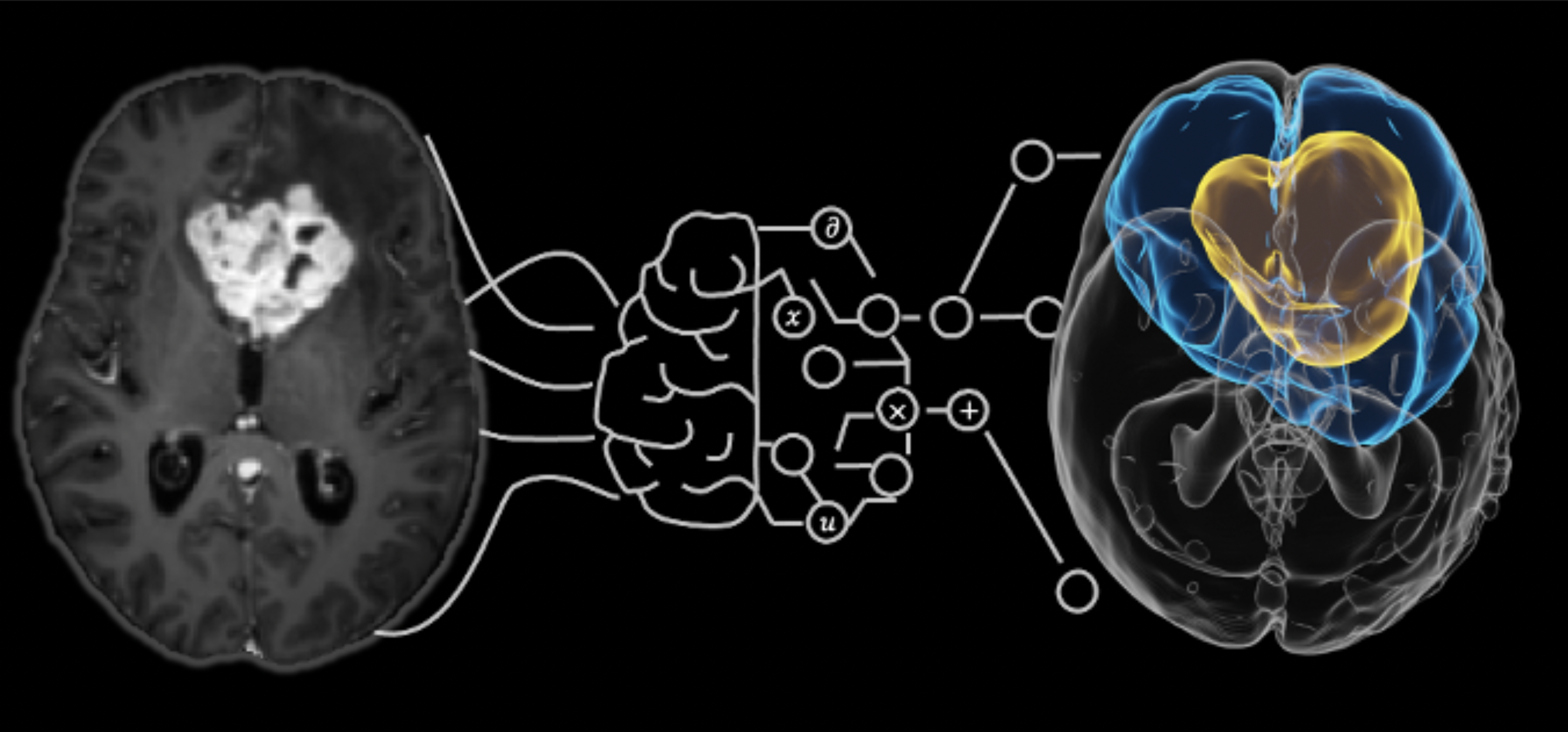
On the left, a brain MRI scan that showcases the tumor region. On the right, a 3D visualization that predicts tumor growth regions (yellow/blue).
As artificial intelligence (AI) becomes more sophisticated, its applications in scientific research and healthcare continue to expand. At UC Irvine, Ray Zhang, a visiting assistant professor in the Department of Mathematics, is harnessing AI to push the boundaries of brain cancer research. As an applied mathematician, Zhang is drawn to complex problems and is motivated by how little standard medical scans reveal about the full extent of the disease.
In his research, Zhang uses mathematical and computational methods to study glioblastoma – a common and aggressive form of brain tumor. Glioblastomas account for approximately 14 percent of all brain tumors, and are particularly difficult to treat because they grow rapidly and invade nearby brain tissue. This invasion makes it virtually impossible to completely remove the tumors; nearly all glioblastoma tumors recur after treatment, and the 5-year survival rate for glioblastomas is just 6.9 percent, according to the National Brain Tumor Society – a figure that has not improved in decades. Over the past century, only four drugs and one medical device have been approved by the FDA to treat glioblastomas, underscoring the need for more innovative treatment options.
Zhang, who received his Ph.D. in Mathematics from UC San Diego, believes AI can help doctors design better treatment plans. “AI's power lies in its ability to identify patterns from massive amounts of data – far beyond what humans could process manually – and integrate data of very different types such as genomic, image scans and family history,” said Zhang. “With the amount of medical data that is available, AI can uncover hidden insights that are difficult, or impossible, for humans to find unaided.”
Despite the potential for breakthroughs, there are significant challenges. High-quality medical data, especially imaging scans for brain tumors or neurodegenerative diseases, remain scarce and expensive to collect. Relying solely on population-level data—which may be limited or non-representative—might lead to biased or unreliable predictions. “That’s why we emphasize patient-specific mathematical modeling, which allows us to go beyond the data and incorporate underlying biological principles to improve generalizability,” Zhang notes.
Zhang collaborates with Dr. John Lowengrub, professor of mathematics and biomedical engineering professor at UC Irvine. Lowengrub’s team has long used mathematical and computational models in cancer research, with the goal of maximizing treatment effectiveness while minimizing patient suffering.
“To predict how far tumor cells have infiltrated surrounding brain tissue, we use machine learning algorithms that combine mathematical models of tumor growth with data from standard-of-care medical images,” says Lowengrub. “This is a novel approach for accurately estimating patient-specific predictions that may improve radiotherapy planning. Knowing the extent of infiltration and the density of tumor cells, we can target cancer cells more precisely while sparing healthy tissue.”
Treatments for glioblastoma, including surgery, radiation and chemotherapy, come at a steep cost and can lead to financial hardships for families. Since the treatments afflict the brain itself, they can inadvertently damage healthy brain tissues and cause the patient to lose their cognitive skills and control of their mood and behavior.
Looking ahead, Zhang and Lowengrub are optimistic about the future of AI in cancer care. “AI tools are already being used to analyze tissue images to detect cancer cells, estimate patient survival based on tumor properties and identify new drugs,” said Lowengrub. “Combining the statistical power of machine learning with the interpretability and predictive strength of biophysical models will enable the development of more robust, patient-specific tools for diagnosis, prognosis and treatment planning in cancer.”
This article was written by Ph.D. student Jenny Tran from the UC Irvine Department of Chemistry. Tran is a 2024-2025 UC Irvine School of Physical Sciences Science Communication Fellow.